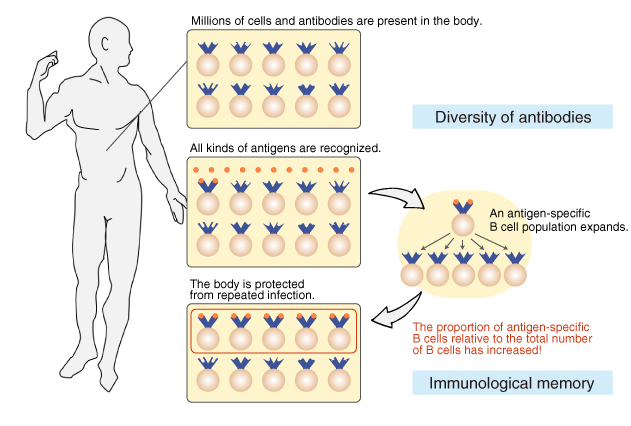
With a full-length protein antigen there will typically be multiple B cells generating antibodies against multiple epitopes from different regions of the protein. Antibodies are produced by a type of white blood cell called a B cell B lymphocyte.
 Kyowa Kirin Therapeutic Antibodies Preparation Of Therapeutic Antibody
Kyowa Kirin Therapeutic Antibodies Preparation Of Therapeutic Antibody
It is the production site for antibodies that is activated in the presence of a particular antigen.
Where are antibodies produced. The variable region of the heavy chain differs in antibodies produced by different B cells but is the same for all antibodies produced by a single B cell or B cell clone. Antibodies also called immunoglobulins or gamma-globulins are made in a type of white blood cell called B-cells. The animal is immunized repeatedly to obtain higher titers of antibodies specific for the antigen.
The variable region of each heavy chain is approximately 110 amino acids long and is composed of a single Ig domain. When activated the B cells develop into plasma cells that generate the antibodies. B cells develop from stem cells in bone marrow.
Antibodies are produced by specialized white blood cells called B lymphocytes or B cells. A negative result means no while borderline results are considered inconclusive. The resulting hybridoma cells are cultured and continue to produce antibodies to the antigen.
How many antibodies are produced. The mature B cells called plasma cells secrete millions of antibodies into the bloodstream and lymphatic system. There are several different kinds of antibodies and typically vaccines are designed to produce the antibodies that recognize and tag viruses as foreign invaders by binding to unique parts of a virus.
Antibodies bind to specific antigens on pathogens. Antibodies being produced from another animal for a pathogen and are injected into the bloodstream to produce immunity as long as they remain in circulation. Within a few weeks these polyclonal antibodies can be harvested and collected from the antiserum.
This binding can inhibit pathogen infectivity by blocking key extracellular sites such as receptors involved in host cell entry. An antibody is a Y-shaped protein produced by B cells which are part of the immune system. Antibodies arent found anywhere in the body in large numbers but when an antigen belonging to a pathogen binds to the receptors on a B-cellso called because they are formed in the bone marrow this stimulates cell division by mitosis.
Antibodies are produced by plasma cells but once secreted can act independently against extracellular pathogen and toxins. A positive result means yes the test has detected the antibody or antigen. When B cells become activated due to the presence of a particular antigen they develop into plasma cells.
In contrast polyclonal antibodies bind to multiple epitopes and are usually. Monoclonal antibodies mAbs are produced by introducing an antigen to a mouse and then fusing polyclonal B cells from the mouses spleen to myeloma cells. From immune B cells.
Blood isolated from these animals contains polyclonal antibodies multiple antibodies that bind to the same antigenin the serum which can now be called antiserum. A monoclonal antibody mAb or moAb is an antibody made by cloning a unique white blood cellAll subsequent antibodies derived this way trace back to a unique parent cell. These lymphocytes may be from a mouse or rat.
Specific antibodies are produced by injecting an antigen into a mammal such as a mouse rat rabbit goat sheep or horse for large quantities of antibody. Plasma cells create antibodies specific to a certain antigen. These antibodies can then be collected directly in the serum or by isolating the individual B cells that produce antibody against the epitope of interest.
Antibody tests do not detect the actual pathogens that cause an infectionthey detect the antibodies that are produced in response to the infection. In the in vitro method antibodies are produced using the hybridoma method where hybridoma cells are generated by fusing myeloma cells and B-lymphocytes. Polyclonal antibodies are typically produced by injecting an animal with the antigen stimulating an immune response and then extracting the animals plasma to produce antibodies en masse.
The B cell is a type of white blood cell that develops from the stem cells in the bone marrow. They are in the blood stream lymph. When an antigen binds to the B-cell surface it stimulates the B cell to divide and mature into a group of identical cells called a clone.
Monoclonal antibodies can have monovalent affinity binding only to the same epitope the part of an antigen that is recognized by the antibody. Polyclonal antibodies are produced by injecting a specific antigen into lab animals such as rabbits and goats etc.
Lab report for a Positive Hepatitis B Surface Antibody Titer titer. A reactive or positive antibody test means you have been infected with the hepatitis C virus at some point in time.
It is not a routine blood test so it is not likely that you have done it in the past unless needed for another academic health related program or job Remember that the titer documentation is program specific.

Hepatitis a antibodies positive. If the antibody test result is positive you should be tested for hepatitis C RNA see Hepatitis C RNA which determines whether you are chronically infected. Many cases have few or no symptoms especially in the young. Positive results indicate acute or recent.
Some people have antibodies associated with the virus in their blood but do not have an active hepatitis C infection. The lab will perform this RNA test automatically if your hepatitis C antibody test is positive. If you are exposed to hepatitis A your body will first produce hepatitis A IgM antibodies.
A blood sample is taken by needle from a vein in the arm. This is true if they have cleared the virus have been cured or still have the virus in their blood. This test always registers positive when a patient has symptoms and should continue to register positive for four to six months.
The test detects the presence of this antibody. Hepatitis A is an infectious disease of the liver caused by Hepatovirus A HAV. If results from the IgM-specific or from both assays are positive recent infection is suspected.
Normal results are negative or nonreactive meaning that you dont have the hepatitis A IgM in your blood. Cautions Discusses conditions that may cause diagnostic confusion including improper specimen collection and handling inappropriate test selection and interfering substances. However hepatitis A IgM antibody will persist lifelong in the blood and is protective against reinfection.
As required by laws in almost all states positive anti-HAV IgM test results must be urgently reported to state health departments for epidemiologic investigations of possible outbreak transmission. Positive HAV-IgM and positive HAV-IgG acute hepatitis A infection is likely. A positive result usually means that youve been exposed to the hepatitis C virus.
These antibodies typically develop 2 to 3 weeks after first being infected and persist for about 2 to 6 months. Hepatitis C is a viral liver infection that can become chronic. You have had an HAV infection in the last 6 months.
Antibody to Hepatitis A in Serum NHANES 2007-2008 4 Consider all serum specimens for analysis potentially positive for infectious agents including HIV and the hepatitis B virus. How is hepatitis A virus infection prevented. How is this test done.
Assays for total immunoglobulin G and immunoglobulin M IgM hepatitis A antibody and IgM-specific hepatitis A antibody assist in differentiating recent infection from prior exposure. The patients immune system makes antibodies against HAV that confer immunity against future infection. You have an active HAV infection.
When symptoms occur they typically last eight weeks and may include nausea vomiting diarrhea jaundice fever and. People with hepatitis A are advised to. Positive HAV-IgM and negative HAV-IgG IgM result may be a false positive.
The hepatitis C antibody test is a blood test that looks for hepatitis C antibodies in the bloodstream. A high IgG reactivity and a moderate level of IgM suggests hepatitis A infection in the recent past rather than current acute infection. If you test positive for them but not for IgM antibodies it means you had a hepatitis A infection in the past or had vaccinations to protect against it.
Hepatitis A or infectious jaundice is caused by hepatitis A virus HAV a picornavirus transmitted by the fecal-oral route often associated with ingestion of contaminated foodIt causes an acute form of hepatitis and does not have a chronic stage. Wear protective gloves eye wear and lab coat during all steps of this method because of infectious contamination hazards. How is the sample collected for testing.
Hepatitis A antibodies are produced in response to an infection with the hepatitis A virus. The results can be complicated as a positive test does not always mean someone has hepatitis C. The hepatitis C antibody test is the only way to check if a person has had the hepatitis C virus.
Immunoglobulin G antibodies to the hepatitis A virus which appear early in the course of infection provide lifelong protection against the disease. They are usually present 5-6 days prior to onset of symptoms. They protect you against hepatitis A.
If your test is positive or reactive it may mean. Vaccination with the full two-dose series of hepatitis A vaccine is the best way to prevent infection. This is the blood test that checks for immunity to Hepatitis B.
It is a type of viral hepatitis. The test is done with a blood sample. A positive result indicates the presence of HAV-specific IgG antibody from either vaccination or past exposure to hepatitis A virus.
Antibody tests for hepatitis viruses may help determine the cause. The time between infection and symptoms in those who develop them is between two and six weeks. Once people have been infected they will always have antibodies in their blood.
Subsequently they were reported in a large number of cases with type 1 diabetes. This assay is intended for the semi-quantitative determination of the GAD Ab in human CSF.
 Sitagliptin In Glutamic Acid Decarboxylase Antibody Positive Diabetes Mellitus Semantic Scholar
Sitagliptin In Glutamic Acid Decarboxylase Antibody Positive Diabetes Mellitus Semantic Scholar
What is Glutamic Acid Decarboxylase Antibodies GAD 65 Test.
Glutamic acid decarboxylase antibodies. Glutamic Acid Decarboxylase-65 Antibody - Glutamic acid decarboxylase GAD-65 antibody is useful to diagnose insulin dependent diabetes mellitus Type I diabetes autoimmune-mediated diabetes to assess risk for development of Type I diabetes to predict onset of Type I diabetes and risk of development of related endocrine disorders eg thyroiditis. Glutamic acid decarboxylase GAD is the enzyme that catalyses the production of GABA a major neurotransmitter of the central nervous system. Results should be interpreted within the context of clinical symptoms.
Autoantibodies recognising the islet cell antigens glutamic acid decarboxylase GAD 65 Zinc Transporter 8 ZnT8 and the insulinoma antigen 2 IA-2 are present in up to 90 of newly diagnosed patients with type 1 diabetes. This enzyme is responsible for converting glutamic acid to GABAa chemical found in high concentrations in the cerebellum. Glutamic acid decarboxylase GAD is the enzyme responsible for the synthesis of gamma-aminobutyric acid GABA.
The anti-glutamic acid decarboxylase anti-GAD65 antibody recognizes cerebellar neurons reacting with the cytoplasm of Purkinje cells and nerve terminals in both molecular and granular cell layers Solimena et al 1990The antibody also reacts with nerve terminals. Posner in The Autoimmune Diseases Fifth Edition 2014 Anti-Glutamic Acid Decarboxylase. Antibodies against the 65-kDa isoform of glutamic acid decarboxylase GAD 65 can be applied as a predictive tool for childhood type-1 diabetes and to facilitate the differential diagnosis of diabetes in adults However the sensitivity and specificity of GAD antibody screening have not been fully characterized and the positive predictive value of screening varies from 20.
Anti-glutamic acid decarboxylase GAD antibodies. We present two patients who presented with Guillain-Barre GBS. They appear years before the onset of clinical diabetes.
Diabetic patients with polyendocrine disorders also generally have glutamic acid decarboxylase GAD65 antibody values 002 nmolL. Other antibody tests include Islet Antigen-2 IA-2 Autoantibody 3001499 Insulin Antibody 0099228 Islet Cell Cytoplasmic Antibody IgG 0050138 and Zinc Transporter 8 Antibody 2006196. Both isoforms are present in both the brain and pancreas.
Antibodies specific for the 65 kDa isoform of glutamic acid decarboxylase GAD65 comprise the majority of pancreatic islet cell autoantibodies. Antibodies to GAD GAD-Ab were first recognised in a patient affected by stiff-person syndrome. Glutamic Acid Decarboxylase Antibodies test is used to discover whether the patient has Type 1 Diabetes or Latent Autoimmune Diabetes of Adulthood.
Antibodies specific for glutamic acid decarboxylase GAD65 account for most but not all antibodies detected in the islet cell antibody test IA-2. Autoimmunity is a disorder where the bodys immune system attacks their own native cells rather than the. This test allows for the detection of the presence of antibodies to glutamic acid decarboxylase which provides early evidence of autoimmune disease activity.
L-Glutamic acid decarboxylase GAD l-glutamate decarboxylase EC 41115 is the crucial enzyme involved in the synthesis of gamma-aminobutyric acid GABA a major neurotransmitter of the central nervous system CNSIn the presence of pyridoxal 5-phosphate PLP as cofactor GAD catalyzes the irreversible alphadecarboxylation of l-glutamic acid to yield GABA and CO 2. GABA is an important inhibitory neurotransmitter in neurons and beta pancreatic cells. An antibody is a protein that your immune system.
Your pancreas needs the enzyme glutamic acid decarboxylase GAD to function normally. A value greater than 50 IUmL is considered positive for glutamic acid decarboxylase antibody GAD AB CSF. Anti-GAD antibodies target an enzyme called Glutamic Acid Decarboxylase.
Anti-glutamic acid decarboxylase GAD antibodies have been discovered in a variety of neurological syndromes with unique presentations. In most cases use glutamic acid decarboxylase antibody in combination with another antibody test. These syndromes include limbic encephalitis LE stiff person syndrome SPS opsoclonus-myoclonus-ataxia syndrome cerebellar ataxia status epilepticus and palatal myoclonus among others.
Glutamic acid decarboxylase GAD is present in highest concentration in brain and pancreatic beta cells. This test is favoured for which type of diabetes from C- peptide test which measures how much insulin is produced by the body. Its measurement has been shown to be useful in assisting the physician in the prediction diagnosis and management of patients with diabetes.
It is believed that the lack of GABA results in cerebellar ataxia. Antibodies that target this enzyme are called GAD antibodies. Glutamic Acid Decarboxylase GAD is an enzyme that plays an important role in synthesizing an important inhibitory neurotransmitter in the body termed as gamma-aminobutyric acid GABA.
IA-2 a protein tyrosine kinase-like protein insulin and zinc transporter-8 antibodies are complementary islet cell antibodies. The two isoforms in glutamic acid decarboxylase are identified as GAD-67 and GAD-65 2. Paraneoplastic Neurological Syndromes and Glutamic Acid Decarboxylase Antibodies Patients with GAD-abs must be screened for an underlying cancer if they have clinical presentations different from those typically associated with this autoimmunity or develop classic PNS.